Approfondimenti scientifici
Rooming-in 2.0: New frontiers in the birth pathway
Rooming-in—meaning the newborn’s continuous stay in the same room as the mother, 24 hours a day from the first hours of life—is a key approach for promoting both neonatal and maternal health. This practice is not limited to simply placing the baby physically next to the mother: it fosters early and constant contact that supports critical physiological, psychological, and behavioral processes during the postpartum period.

From a physiological perspective, continuous proximity stimulates the release of maternal oxytocin, which is essential not only for postpartum uterine contractions and bleeding control, but also for facilitating early milk “coming in” and sustaining milk production over time. For the newborn, direct contact with the mother regulates the autonomic nervous system, lowering cortisol levels, improving thermoregulation, and stabilizing heart rate and breathing. In addition, rooming-in helps mothers learn neonatal cues, improving their ability to recognize hunger and sleep signals—an essential element for initiating effective breastfeeding and building a secure emotional bond.
On a psychological level, continuous rooming-in strengthens perceived maternal competence (maternal self-efficacy), reduces postpartum anxiety and stress, and promotes sensitive, responsive caregiving behaviors. Clinical studies have shown that mothers who adopt rooming-in demonstrate greater confidence in newborn care, higher postpartum satisfaction, and better indicators of mother–infant interaction, with positive long-term effects on the newborn’s socio-emotional development.
Rooming-in and the promotion of breastfeeding
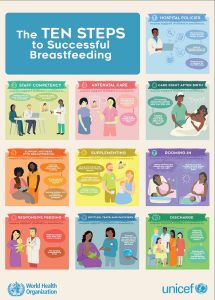
Rooming-in also fits within international strategies to promote breastfeeding, as outlined in the UNICEF/WHO “Ten Steps to Successful Breastfeeding,” where continuous mother–infant proximity is a cross-cutting component that directly influences early initiation, feeding frequency, and the duration of exclusive breastfeeding. Widespread adoption of rooming-in therefore represents not only an organizational measure, but a true clinical intervention supported by consolidated scientific evidence (Fig.1).
Despite its many benefits, rooming-in must be implemented with careful attention to safety—especially in the first hours of life and during the night—to prevent risks such as falls or episodes of sudden unexpected postnatal collapse, through appropriate protocols, staff training, and maternal education.
Physiological and behavioral benefits of rooming-in
- Neuroendocrine regulation
Continuous proximity increases maternal oxytocin release, promoting:
-
- effective postpartum uterine contractions,
- emotional stabilization,
- greater milk ejection.
In the newborn, contact with the mother modulates the stress axis (HPA), reducing cortisol and improving thermoregulation and cardio-respiratory stability.
- Early initiation and maintenance of breastfeeding
Rooming-in supports interpretation of neonatal cues (movements, rooting, hands to mouth), promoting feeding on demand, which is associated with:
-
- greater milk production,
- longer breastfeeding duration,
- fewer unnecessary supplements.
Clinical studies show that mother–newborn separation in the first hours of life compromises the start of effective sucking and reduces exclusive breastfeeding rates in subsequent weeks.
- Newborn physiological stability
Rooming-in contributes to stability in:
-
- blood glucose,
- temperature,
- cardio-respiratory function,
- immune function, thanks to increased skin-to-skin contact and early intake of colostrum.
- Strengthening the mother–infant relationship
Continuous interaction helps the mother develop competence and confidence in newborn care (maternal self-efficacy), a protective factor against postpartum anxiety and depression.
The “UNICEF Ten Steps to Successful Breastfeeding” and the central role of rooming-in
UNICEF and WHO define ten evidence-based steps that support breastfeeding and the mother–infant relationship. Rooming-in is directly linked to several of these steps:
- Have written breastfeeding policies that are known to all staff.
- Train healthcare staff to implement the necessary skills.
- Inform all mothers about the benefits and management of breastfeeding.
- Support the initiation of breastfeeding within the first hour of life.
- Show mothers how to breastfeed and how to maintain milk production even if they are separated from their baby.
- Do not give foods or fluids other than breast milk unless medically indicated.
- Enable continuous room-sharing between mother and newborn (rooming-in) 24 hours a day.
- Encourage feeding on demand.
- Do not give teats/nipples or pacifiers to breastfed newborns.
- Promote continuity of care through community networks and post-discharge support.
The link between rooming-in and the Ten Steps
Rooming-in is a cross-cutting element supporting multiple goals:
- Enables early initiation of breastfeeding (Step 4).
- Facilitates maternal learning about latch, sucking, and positions (Step 5).
- Promotes exclusive, on-demand breastfeeding (Step 8).
- Reduces unnecessary supplementation (Step 6).
- Improves parental competence and reduces unnecessary medicalization.
In this sense, it is not merely an organizational act, but an evidence-based clinical intervention that is essential for breastfeeding physiology (Fig. 2).
Rooming-in as a multidimensional strategy
Rooming-in is confirmed as a multidimensional strategy capable of positively influencing multiple maternal–newborn health outcomes. Beyond well-established benefits for breastfeeding and bonding, it contributes to consolidating parenting skills, supports the newborn’s physiological adaptation, and promotes a family-centered care environment. Continuous rooming-in also facilitates early observation of any clinical or physiological signs in the newborn, enabling timely interventions, and supports continuity of care between the hospital ward and discharge, integrating with community networks that support mothers and infants.
From a health policy perspective, systematic implementation of rooming-in is an indicator of the quality of postpartum care, as it reflects the system’s ability to combine safety, clinical effectiveness, and the promotion of psychological well-being. Widespread adoption of this practice can help reduce unnecessary interventions, encourage responsive caregiving behaviors, and create a model of care centered on the mother–infant relationship.
Finally, although scientific data confirm numerous advantages, areas remain where further research is needed: the impact of rooming-in on long-term outcomes, optimal strategies for nighttime surveillance, and its role in high-risk contexts (mothers with post-cesarean analgesia or complex medical conditions). Continued production of high-quality evidence may refine clinical guidelines, optimize safety protocols, and consolidate rooming-in as a standardized, universal practice capable of maximizing benefits for mothers, newborns, and healthcare systems.
Bergman NJ. Birth practices: Maternal-neonate separation as a source of toxic stress.
Birth Defects Res. 2019;111(15):1087-1109
British Association of Perinatal Medicine (BAPM). Sudden and Unexpected Postnatal
Collapse: A BAPM Framework for Reducing Risk, Investigation and Management. May
- https://www.bapm.org/resources/sudden-and-unexpected-postnatal-collapse-supc
Comitato Percorso Nascita Nazionale (CPNn) 2010. Accordo del 16 dicembre 2010, ai sensi dell’articolo 9 del decreto legislativo 28 agosto 1997, n. 281, tra il Governo, le regioni e le province autonome di Trento e Bolzano, le province, i comuni e le comunità montane sul documento concernente «Linee di indirizzo per la promozione ed il miglioramento della qualità, della sicurezza e dell’appropriatezza degli interventi assistenziali nel percorso nascita e per la riduzione del taglio cesareo». (Rep. atti n. 137/CU) (11A00319). (G.U. Serie Generale , n. 13 del 18 gennaio 2011)
Davanzo R, Maffeis C, Silano M, Bertino E, Agostoni C, Cazzato T, Tonetto P, Staiano A,
Vitiello R, Natale, Gruppo di Lavoro ad hoc. Allattamento al seno e uso del latte materno/umano Position Statement 2015. SIP, SIN, SICuPP, SIGENP e SIMP. https://www.salute.gov.it/imgs/C_17_pubblicazioni_2415_allegato.pdf 5.
Davanzo R, Mosca F. Allattamento e infezione da SARS-CoV-2. Medico e Bambino 2020;39(4):241-242 6.
Davanzo R, Risso F. L’assistenza al neonato fisiologico in ospedale: coniugare sicurezza e promozione della salute. Medico e Bambino 2020;39:35-44
Decreto del Presidente della Repubblica 14 gennaio 1997. Approvazione dell’atto di indirizzo e coordinamento alle regioni e alle province autonome di Trento e di Bolzano, in materia di requisiti strutturali, tecnologici ed organizzativi minimi per l’esercizio delle attività sanitarie da parte delle strutture pubbliche e private. (GU Serie Generale n.42 del 20-02-1997 – Suppl. Ordinario n. 37)
Giusti A, Chapin EM, Spila Alegiani S, Marchetti F, Sani S, Preziosi J, Colaceci S, Zambri F.
Prevalence of breastfeeding and birth practices during the first wave of the COVID-19 pandemic within the Italian Baby-Friendly Hospital network. What have we learned? Ann Ist Super Sanita. 2022 Apr-Jun;58(2):100-108
Istituto Superiore di Sanità- ISS EpiCentro, Sorveglianza Bambini 0-2 anni, https://www.epicentro.iss.it/sorveglianza02anni/indagine-2022- risultati?utm_source=newsletter&utm_medium=email&utm_campaign=30marzo2023
https://www.epicentro.iss.it/sorveglianza02anni/pdf/Sintesi_CONVEGNO-O_2__Versione%20STAMPA_23_Marzo_2023.pdf
Ministero della Salute (2014). Raccomandazione per la prevenzione della morte o disabilità permanente in neonato sano di peso> 2500 grammi non correlata a malattia congenita. Direzione Generale della Programmazione Sanitaria (DGPROG). Aprile 2014; https://www.salute.gov.it/imgs/C_17_pubblicazioni_2157_allegato.pdf 25.
Ministero della Salute (2017). Comitato Percorso Nascita. Linee di indirizzo per la definizione e l’organizzazione dell’assistenza in autonomia da parte delle ostetriche alla gravidanza a basso rischio ostetrico (BRO). DGPROG/DGPREV. 23 ottobre 2017 26.
Ministero della Salute (2021); Tavolo Tecnico Allattamento (TAS). La continuità del rapporto madre-bambino e il mantenimento dell’allattamento in caso di ricovero ospedaliero.
Indicazioni a cura del Gruppo di Lavoro multi-professionale 2020-2021. Ministero della Salute, 3 maggio 2021 27.
Ministero della Salute (2023). Allattamento e promozione della salute materno-infantile: focus sulla salute mentale. Position Statement di TAS, UNICEF, Società Italiana di Psichiatria, Società Italiana di Neurologia, Lega Italiana contro l’Epilessia (LICE), Società Italiana di Neuropsichiatria dell’Infanzia e dell’Adolescenza (SINPIA), Ordine Psicologi del Lazio, Associazione Epilessia (AE), Associazione Italiana Sclerosi Multipla (AISM), Fondazione ONDA e Vivere Onlus. 11 febbraio 2023 28.
Ministero della Salute. (2019). Investire precocemente in salute: azioni e strategie nei primi mille giorni di vita. Documento di indirizzo per genitori, operatori sanitari e policy maker, per la protezione e promozione della salute dei bambini e delle generazioni future. Tavolo tecnico “Investire precocemente in salute: azioni e strategie nei primi mille giorni di vita” Documento di indirizzo per genitori, operatori sanitari e policy maker, per la protezione e promozione della salute dei bambini e delle generazioni future. DGPREV-MDS, 12 luglio 2019
MINISTERO DELLA SALUTE https://www.pnrr.salute.gov.it/imgs/C_17_pubblicazioni_3477_allegato.pdf
NICE-National Institute of Clinical Excellence. Antenatal Care, 19 August 2021. https://www.nice.org.uk/guidance/ng201 32.
NICE. Intrapartum care. Quality standard [QS105]. Published: 10 December 2015. Last updated: 28 February 2015. https://www.nice.org.uk/guidance/qs105/chapter/quality-statement-7-skin-to-skin-contact
SIN, SIP, SIGO, AOGOI, FNOPO, AGUI, SIMP, SININF, FNOPI, Vivere Onlus (2021), Standard Organizzativi per l’Assistenza Perinatale. IdeaCPA Editore, Roma 2021 37.
SIN, SIP, SIGO, SINUPE, AOGOI, FNOPO, FNOPI, SININF, SIPINF e VIVERE ONLUS (2023). Politica aziendale sull’allattamento (PAA). Un progetto inter-societario di promozione della salute materno-infantile. 2 febbraio 2023 38.
Sistema Nazionale per le Linee Guida (SNLG). Istituto Superiore di Sanità. Gravidanza Fisiologica. Aggiornamenti 2011. https://www.salute.gov.it/imgs/C_17_pubblicazioni_1436_allegato.pdf
Società Italiana Neonatologia. Standard Organizzativi per l’Assistenza Perinatale. Edizione maggio 2021, IdeaCpa Editore, Roma. ISBN 978-88-946-318-90
Tavolo tecnico in materia di tutela e promozione della salute nei primi 1000 giorni di vita: dal concepimento ai due anni di età, Direzione generale della prevenzione sanitaria, Ministero della Sanità. Investire precocemente in salute: azioni e strategie nei primi mille giorni di vita. https://www.salute.gov.it/imgs/C_17_pubblicazioni_3120
Task Force SUPC della Società Italiana di Neonatologia. Indicazioni sulla prevenzione e gestione del collasso Postnatale (SUPC). Edizione marzo 2023.
World Health Organization & United Nations Children’s Fund (UNICEF). (2018).
Implementation guidance: protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services: the revised baby-friendly hospital initiative. World Health Organization. https://apps.who.int/iris/handle/10665/272943.
License: CC BY-NC-SA 3.0 IGO
